PassMaker
A pacemaker is a small device placed in your chest. It helps control your heartbeat. You may need a pacemaker if your heartbeat is too slow, too fast, or irregular. A pacemaker is about the size of a large wristwatch. A Simple Word Count Planner for Writers, Students and Nanowrimo Participants. Pacemaker is a Simple Flexible Goal Planner for Writers & Students. Give a memorable name to your project and determine how much you want to do within your timeframe. Pacemaker has been around since 2004 and is a collaborative effort by the ClusterLabs community, including full-time developers with Red Hat and SuSE. Pacemaker ships with most modern Linux distributions and has been deployed in many critical environments including Deutsche Flugsicherung GmbH ( DFS ) which uses Pacemaker to ensure its air.
What is a pacemaker insertion?
A pacemaker insertion is the implantation of a small electronic device that is usually placed in the chest (just below the collarbone) to help regulate slow electrical problems with the heart. A pacemaker may be recommended toensure that the heartbeat does not slow to a dangerously low rate.
The heart's electrical system
The heart is basically a pump made up of muscle tissue that is stimulated by electrical currents, which normally follow a specific circuit within the heart.
This normal electrical circuit begins in the sinus or sinoatrial (SA) node, which is a small mass of specialized tissue located in the right atrium(upper chamber) of the heart. The SA node generates an electrical stimulus at 60 to 100 times per minute (for adults) under normal conditions; this electrical impulse from the SA node starts the heartbeat.
The electrical impulse travels from the SA node via the atria to the atrioventricular (AV) node in the bottom of the right atrium. From there the impulse continues down an electrical conduction pathway called the Bundle of His and then on through the 'His-Purkinje' system into the ventricles (lower chambers) of the heart. When the electrical stimulus occurs it causes the muscle to contract and pump blood to the rest of the body. This process of electrical stimulation followed by muscle contraction is what makes the heart beat.
A pacemaker may be needed when problems occur with the electrical conduction system of the heart. When the timing of the electrical stimulation of the heart to the heart muscle and the subsequent response of the heart's pumping chambers is altered, a pacemaker may help.
What is a pacemaker?
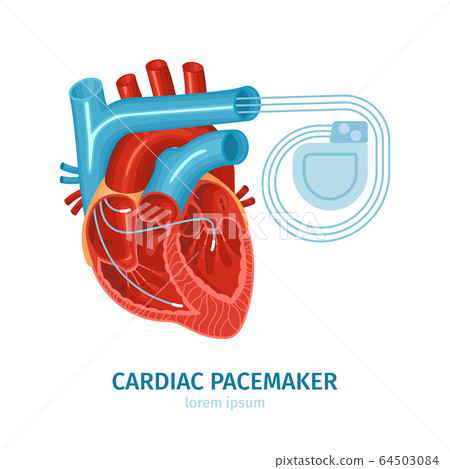
A pacemaker is composed of three parts: a pulse generator, one or more leads, and an electrode on each lead. A pacemaker signals the heart to beat when the heartbeat is too slow or irregular.
A pulse generator is a small metal case that contains electronic circuitry with a small computer and a battery that regulate the impulses sent to the heart.
The lead (or leads) is an insulated wire that is connected to the pulsegenerator on one end, with the other end placed inside one of the heart'schambers. The lead is almost always placed so that it runs through a largevein in the chest leading directly to the heart. The electrode on the endof a lead touches the heart wall. The lead delivers the electrical impulsesto the heart. It also senses the heart's electrical activity and relaysthis information back to the pulse generator. Pacemaker leads may bepositioned in the atrium (upper chamber) or ventricle (lower chamber) orboth, depending on the medical condition.
If the heart's rate is slower than the programmed limit, an electricalimpulse is sent through the lead to the electrode and causes the heart tobeat at a faster rate.
When the heart beats at a rate faster than the programmed limit, thepacemaker generally monitors the heart rate and will not pace. Modernpacemakers are programmed to work on demand only, so they do not competewith natural heartbeats. Generally, no electrical impulses will be sent tothe heart unless the heart's natural rate falls below the pacemaker's lowerlimit.
Pacemaker Defibrillator
A newer type of pacemaker, called a biventricular pacemaker, is currentlyused in the treatment of specific types of heart failure. Sometimes inheart failure, the two ventricles do not pump in a normal manner.Ventricular dyssynchrony is a common term used to describe this abnormalpumping pattern. When this happens, less blood is pumped by the heart. Abiventricular pacemaker paces both ventricles at the same time, increasingthe amount of blood pumped by the heart. This type of treatment is calledcardiac resynchronization therapy or CRT.
After a pacemaker insertion, regularly scheduled appointments will be madeto ensure the pacemaker is functioning properly. The doctor uses a specialcomputer, called a programmer, to review the pacemaker's activity andadjust the settings when needed.
Other related procedures that may be used to assess the heart includeresting and exerciseelectrocardiogram (ECG), Holter monitor, signal-averaged ECG,cardiac catheterization,chest X-ray,computed tomography (CT scan) of the chest,echocardiography,electrophysiology studies,magnetic resonance imaging (MRI) of the heart,myocardial perfusion scan (stress),myocardial perfusion scan (resting),radionuclide angiography, andcardiac CT scan. Please see these procedures for additional information. Note thatalthough an MRI is a very safe procedure, the magnetic fields used by theMRI scanner may interfere with the pacemaker's function. Any patient with apacemaker should always speak with his or her cardiologist beforeundergoing an MRI.
Reasons for the procedure
A pacemaker may be inserted in order to stimulate a faster heart rate whenthe heart is beating too slowly, and causing problems that cannot otherwisebe corrected.
Problems with the heart rhythm may cause difficulties because the heart isunable to pump an adequate amount of blood to the body. If the heart rateis too slow, the blood is pumped too slowly. If the heart rate is too fastor too irregular, the heart chambers are unable to fill up with enoughblood to pump out with each beat. When the body does not receive enoughblood, symptoms such as fatigue, dizziness, fainting, and/or chest pain mayoccur.
Some examples of heart rate and rhythm problems for which a pacemaker mightbe inserted include:
Bradycardia. This occurs when the sinus node causes the heart to beat too slowly.
Tachy-brady syndrome. This is characterized by alternating fast and slow heartbeats.
Heart block. This occurs when the electrical signal is delayed or blocked after leaving the SA node; there are several types of heart blocks.

There may be other reasons for your doctor to recommend a pacemakerinsertion.
Risks of the procedure
Possible risks of pacemaker include, but are not limited to, the following:

Bleeding from the incision or catheter insertion site
Damage to the vessel at the catheter insertion site
Infection of the incision or catheter site
Pneumothorax. If the nearby lung is inadvertently punctured during the procedure, leaking air becomes trapped in the pleural space (outside the lung but within the chest wall); this can cause breathing difficulties and in extreme cases may cause the lung to collapse.
If you are pregnant or suspect that you may be pregnant, you should notifyyour health care provider. If you are breastfeeding, you should notify yourhealth care provider.
Patients who are allergic to or sensitive to medications or latex shouldnotify their doctor.
For some patients, having to lie still on the procedure table for thelength of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Besure to discuss any concerns with your doctor prior to the procedure.
Before the procedure
Your doctor will explain the procedure to you and offer you the opportunityto ask any questions that you might have about the procedure:
You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is not clear.
Notify your doctor if you are sensitive to or are allergic to any medications, iodine, latex, tape, or anesthetic agents (local and general).
You will need to fast for a certain period of time prior to the procedure. Your doctor will notify you how long to fast, usually overnight.
If you are pregnant or suspect that you are pregnant, you should notify your doctor.
Notify your doctor of all medications (prescription and over-the-counter) and herbal or other supplements that you are taking.
Notify your doctor if you have heart valve disease, as you may need to receive an antibiotic prior to the procedure.
Notify your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop some of these medications prior to the procedure.
Your doctor may request a blood test prior to the procedure to determine how long it takes your blood to clot. Other blood tests may be done as well.
You may receive a sedative prior to the procedure to help you relax. If a sedative is given and there is a possibility that you may be discharged, you will need someone to drive you home. You will likely spend at least one night in the hospital after the procedure for observation and to ensure the pacemaker functions properly.
Based on your medical condition, your doctor may request other specific preparation.
During the procedure
A pacemaker may be performed on an outpatient basis or as part of your stayin a hospital. Procedures may vary depending on your condition and yourdoctor's practices.
Generally, a pacemaker insertion follows this process:
You will be asked to remove any jewelry or other objects that may interfere with the procedure.
You will be asked to remove your clothing and will be given a gown to wear.
You will be asked to empty your bladder prior to the procedure.
If there is excessive hair at the incision site, it may be clipped off.
An intravenous (IV) line will be started in your hand or arm prior to the procedure for injection of medication and to administer IV fluids, if needed.
You will be placed on your back on the procedure table.
You will be connected to an electrocardiogram (ECG or EKG) monitor that records the electrical activity of the heart and monitors the heart during the procedure using small, adhesive electrodes. Your vital signs (heart rate, blood pressure, breathing rate, and oxygenation level) will be monitored during the procedure.
Large electrode pads will be placed on the front and back of the chest.
You will receive a sedative medication in your IV before the procedure to help you relax. However, you will likely remain awake during the procedure.
The pacemaker insertion site will be cleansed with antiseptic soap.
Sterile towels and a sheet will be placed around this area.
A local anesthetic will be injected into the skin at the insertion site.
Once the anesthetic has taken effect, the physician will make a small incision at the insertion site.
A sheath, or introducer, is inserted into a blood vessel, usually under the collarbone. The sheath is a plastic tube through which the pacer lead wire will be inserted into the blood vessel and advanced into the heart.
It will be very important for you to remain still during the procedure so that the catheter does not move out of place and to prevent damage to the insertion site.
The lead wire will be inserted through the introducer into the blood vessel. The doctor will advance the lead wire through the blood vessel into the heart.
Once the lead wire is inside the heart, it will be tested to verify proper location and that it works. There may be one, two, or three lead wires inserted, depending on the type of device your doctor has chosen for your condition. Fluoroscopy, (a special type of X-ray that will be displayed on a TV monitor), may be used to assist in testing the location of the leads.
The pacemaker generator will be slipped under the skin through the incision (just below the collarbone) after the lead wire is attached to the generator. Generally, the generator will be placed on the nondominant side. (If you are right-handed, the device will be placed in your upper left chest. If you are left-handed, the device will be placed in your upper right chest).
Dont starve together for mac. The ECG will be observed to ensure that the pacer is working correctly.
The skin incision will be closed with sutures, adhesive strips, or a special glue.
A sterile bandage or dressing will be applied.
After the procedure
In the hospital
After the procedure, you may be taken to the recovery room for observationor returned to your hospital room. A nurse will monitor your vital signs.
You should immediately inform your nurse if you feel any chest pain ortightness, or any other pain at the incision site.
After the period of bed rest has been completed, you may get out of bedwith assistance. The nurse will assist you the first time you get up, andwill check your blood pressure while you are lying in bed, sitting, andstanding. You should move slowly when getting up from the bed to avoid anydizziness from the period of bedrest.
You will be able to eat or drink once you are completely awake.
The insertion site may be sore or painful. Pain medication may beadministered if needed.
Your doctor will visit with you in your room while you are recovering. Thedoctor will give you specific instructions and answer any questions you mayhave.
Once your blood pressure, pulse, and breathing are stable and you arealert, you will be taken to your hospital room or discharged home.
If the procedure is performed on an outpatient basis, you may be allowed toleave after you have completed the recovery process. However, it is commonto spend at least one night in the hospital after pacemaker implantationfor observation.
You should arrange to have someone drive you home from the hospitalfollowing your procedure.
At home
You should be able to return to your daily routine within a few days. Yourdoctor will tell you if you will need to take more time in returning toyour normal activities. You should not do any lifting or pulling onanything for a few weeks. You may be instructed to limit movement of thearm on the side that the pacemaker was placed, based on your doctor'spreferences.
You will most likely be able to resume your usual diet, unless your doctorinstructs you differently.
It will be important to keep the insertion site clean and dry. You will begiven instructions about bathing and showering.
Pacemaker Surgery
Your doctor will give you specific instructions about driving.
Ask your doctor when you will be able to return to work. The nature of youroccupation, your overall health status, and your progress will determinehow soon you may return to work.
Notify your doctor to report any of the following:
Fever and/or chills
Increased pain, redness, swelling, or bleeding or other drainage from the insertion site
Chest pain/pressure, nausea and/or vomiting, profuse sweating, dizziness and/or fainting
Palpitations
Your doctor may give you additional or alternate instructions after theprocedure, depending on your particular situation.
Pacemaker precautions
The following precautions should always be considered. Discuss thefollowing in detail with your doctor, or call the company that made yourdevice:
Always carry an ID card that states you have a pacemaker. In addition, you may want to wear a medical identification bracelet indicating that you have a pacemaker.
Let screeners know you have a pacemaker before going through airport security detectors. In general airport detectors are safe for pacemakers, but the small amount of metal in the pacemaker and leads may set off the alarm. If you are selected for additional screening by hand-held detector devices, politely remind the screeners that the detector wand should not be held over your pacemaker for longer than a few seconds, as these devices contain magnets and thus may affect the function or programming of your pacemaker.
You may not have a magnetic resonance imaging (MRI) procedure (unless you have a specially designed pacemaker). You should also avoid large magnetic fields such as power generation sites and industrial sites such as automobile junkyards that use large magnets.
Abstain from diathermy (the use of heat in physical therapy to treat muscles).
Turn off large motors, such as cars or boats, when working close to them as they may create a magnetic field.
Avoid high-voltage or radar machinery, such as radio or television transmitters, electric arc welders, high-tension wires, radar installations, or smelting furnaces.
If you are having a surgical procedure performed, inform your surgeon that you have a pacemaker well before the operation. Also ask your cardiologist's advice on whether anything special should be done prior to and during the surgery, as the electrocautery device that controls bleeding may interfere with the pacemaker. Sometimes the pacemaker's programming will be temporarily changed (using a magnet) during the surgery to minimize the possibility of interference from the electrocautery.
When involved in a physical, recreational, or sporting activity, protect yourself from trauma to the pacemaker. A blow to the chest near the pacemaker can affect its functioning. If you are hit in that area, you may want to see your doctor.
Cell phones in the U.S. with less than 3 watts of output do not seem to affect pacemakers or the pulse generator, but as a precaution, cell phones should be kept at least 6 inches away from your pacemaker. Avoid carrying a cell phone in your breast pocket over your pacemaker.
Always consult your doctor when you feel ill after an activity, or when you have questions about beginning a new activity.
Always consult your doctor if you have any questions concerning the use of certain equipment near your pacemaker.
Internal phone numbers. This material must not be used for commercial purposes, or in any hospital or medical facility. Failure to comply may result in legal action.
Medically reviewed by Drugs.com. Last updated on March 4, 2021.
- Care Notes
WHAT YOU NEED TO KNOW:
A pacemaker is a small device placed in your chest. It helps control your heartbeat. You may need a pacemaker if your heartbeat is too slow, too fast, or irregular. A pacemaker is about the size of a large wristwatch. It is made up of flexible wires (leads) with sensors, a battery, pulse generator, and a small computer. The sensors measure your heartbeat. They send this information to the computer. The computer causes the generator to send electrical impulses to your heart. This makes your heart beat correctly. Some pacemakers can also record your heart rate and rhythm.
DISCHARGE INSTRUCTIONS:
Call 911 for any of the following:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You feel weak, dizzy, or faint.
- Your stitches come apart.
- Your pulse is lower or higher than your healthcare provider said it should be.
Contact your healthcare provider if:
- You have a fever or chills.
- Your wound is red, swollen, or draining pus.
- You have questions or concerns about your condition or care.
Care for your incision as directed:
Ask your healthcare provider when you can remove your bandage. Wash around your incision with soap and water. It is okay to let soap and water run over your incision. Do not scrub your incision. Gently pat the area dry, and apply new, clean bandages as directed. Check your incision every day for redness, swelling, or pus.
Activity:
- Do not lift anything heavier than 3 pounds with the arm closest to your pacemaker. Do not lift the arm over your head until your healthcare provider says it is okay. Ask your healthcare provider how long to follow these instructions.
- Do not do vigorous activities. This includes contact sports and some types of exercise. These activities can damage your pacemaker or cause your wires to move. Ask your healthcare provider what activities are safe for you to do.
Pacemaker safety:
- Tell all healthcare providers that you have a pacemaker. MRI machines and certain equipment used during surgery can affect how your pacemaker works.
- Limit or avoid close contact with certain electrical devices. Examples include cell phones, iPods™, microwave ovens, and generators. These devices can prevent your pacemaker from working correctly. Stand at least 2 feet from a generator. Do not put your cell phone or iPod in the chest pocket closest to your pacemaker. Use the arm opposite your pacemaker to hold and use your cell phone.
- Tell airport security that you have a pacemaker before you go through the metal detectors. Metal detectors may beep because of the metal in your pacemaker. Step away from the machine if you feel dizzy or your heart rate increases. Ask the security agents not to hold a security wand over your pacemaker for more than a few seconds. Your pacemaker function or programming may be affected by the wand.
- Wear medical alert identification. Wear medical alert jewelry or carry a card that says you have a pacemaker. Ask your healthcare provider where to get these items.
- Check your pulse as directed. Check for 1 minute while you are resting. Write down your heart rate. Bring a copy of these numbers to your follow-up visits.
What you need to know about care of your pacemaker:
- Your healthcare provider will check your pacemaker about every 3 months. Some checks may be done over the telephone. He or she will make sure it is working correctly. You may also need regular EKGs to check the electrical activity of your heart.
- Your pacemaker generator, battery, and leads will need to be replaced. The battery may need to be replaced in 6 to 7 years or longer. The generator will be replaced at the same time. The battery and generator are replaced during surgery. Your leads will need to be replaced if they cause an infection or move out of place. Your healthcare provider will monitor you and decide when these parts need to be replaced.

Follow up with your healthcare provider as directed:
Write down your questions so you remember to ask them during your visits.
Pacemakers For The Heart
© Copyright IBM Corporation 2021 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes. All illustrations and images included in CareNotes® are the copyrighted property of A.D.A.M., Inc. or IBM Watson Health
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Natural Pacemaker Of The Heart
Further information
Pacemaker
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
